Best Treatment for Sudden Massive Subretinal Bleeds in Age Related Macular Degeneration
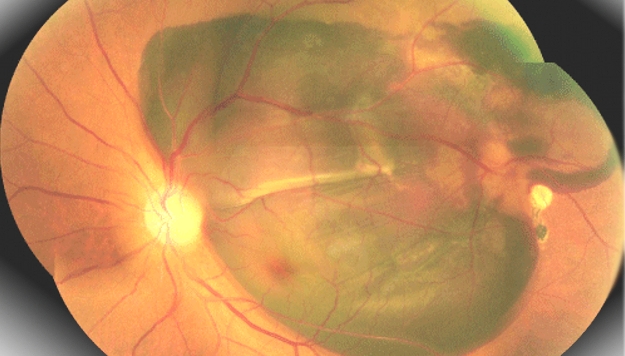
I would like to bring to your attention a recent study published in this month’s Retinal Journal ref¹. This is an interesting article which has tried to compare three different treatment modalities for a group of patients who have a severe (tough reasonably rare) complication of wet macular degeneration. These patients suffer from a spontaneous sudden subretinal largehaemorrhage, which can result in total sudden central visual loss.There is a need for surgical intervention promptly if one is going to attempt to restore some visual acuity in these individuals and the generally accepted window of opportunity is two weeks. Different surgeons have different perspectives regarding what the best treatment modality of this rare complication is. This study attempted to compare three different techniques:
1. Vitrectomy with subretinal TPA injection
2. Pneumatic displacement with intravitreal TPA injection
3. Pneumatic displacement without any TPA administration
What were the study’s findings?
The study concluded that the groups1 and 2 (ie that had vitrectomy with subretinal TPA or pneumatic displacement with intravitreal TPA) had a significant improvement in their visual acuity compared to pre-op. This compared with the 3rd group (pneumatic displacement without any TPA administration)who had no significant visual improvement. There was also evidence that those that underwent a complete vitrectomy with subretinal TPA had a reduction in the size of the scar that developed as a result of the bleed.
What were the limitations of the study?
Clearly the study was small in only having 39 patients, but this is a rare condition and it can be very difficult to have a significantly large number of individuals in a study so the authors have done well in reviewing 39 cases. The other thing that must be borne in mind is that this was not a randomised trial but was a retrospective case series. Nevertheless, it does give the surgeon information regarding the benefit of prompt intervention with a choice of either complete vitrectomy with subretinal TPA or pneumatic displacement with intravitreal TPA. Certainly in the UK, these techniques would also often be administered at the same time as an anti-VEGF drug such as Avastin in order to try and get the underlying wet macular degeneration as stable as possible. It also clearly indicates that pneumatic displacement of itself will not shift a developing/ developed subretinal clot, which is not entirely unsurprising.
Patients that suffer from sudden large subretinal haemorrhage related to wet macular degeneration are often distressed as they have often lost a very significant amount of vision over a short period of time. Whilst this is a rare and potentially devastating complication, some patients do have very good outcomes provided they are referred and treated promptly. In deciding the individual treatment for the patient, of course one must also factor in the acuity in the fellow eye, and their general state of health. If one undertakes a complete vitrectomy, one generally asks the patient to posture upright to displace any haemorrhage inferiorly, whereas if one does an intravitreal pneumatic displacement with intravitreal TPA, one would generally ask the patient to posture at 45 degrees which is much more challenging particularly for this elderly group of patients.
Ultimately, it would be ideal to have a randomised controlled trial of these different modalities so surgeons can, with confidence, try and establish what the best treatment modality is for this rare but devastating complication of surgery (with a control group of observation alone and analysis of post-outcome quality of life utilities) but in its absence, the study certainly lends evidence that we should be intervening in these patients promptly as we can restore a moderate amount of vision with the correct treatment.
¹TISSUE PLASMINOGEN ACTIVATOR FOR SUBFOVEAL HEMORRHAGE DUE TO AGE-RELATED MACULAR DEGENERATION: Comparison of 3 Treatment Modalities. Retina Volume 36(10) 2016 page 1860 - 1865